
DataRise™ Commercial Drug Reimbursement Data is available for custom orders.
Subscribers now have unprecedented access to virtually all commercial contract reimbursement rates by health plan, provider, and drug. Available commercial drug reimbursement rates include those most commonly administered in physician offices (Part B), such as:
Examples: Administered In-Office
- pembrolizumab (Keytruda®) (Oncology)
- aflibercept (Eyelea®) (Ophthalmology)
- faricimab-svoa (VABYSMO®) (Ophthalmology)
- abatacept (Orencia®) (Rheumatology)
- ocrelizumab (Ocrevus®) (Neurology)
- vedolizumab (ENTYVIO®) (Gastroenterology)
- leuprolide acetate (Urology)
- AND MANY MANY MORE!
Queries are custom searches performed by an Acuvance professional upon request. Turnaround times will be quoted at order, but expect turnaround times of 24 to 72 hours for raw data for most query searches. Analysis is a separate service that can be provided by Coker’s consultants.
If there are more than 1 million results, your data will be accessible via a private online portal. The Unlimited Query Plan is subject to limitations on processing time (24 to 72 hours per health plan ordered).
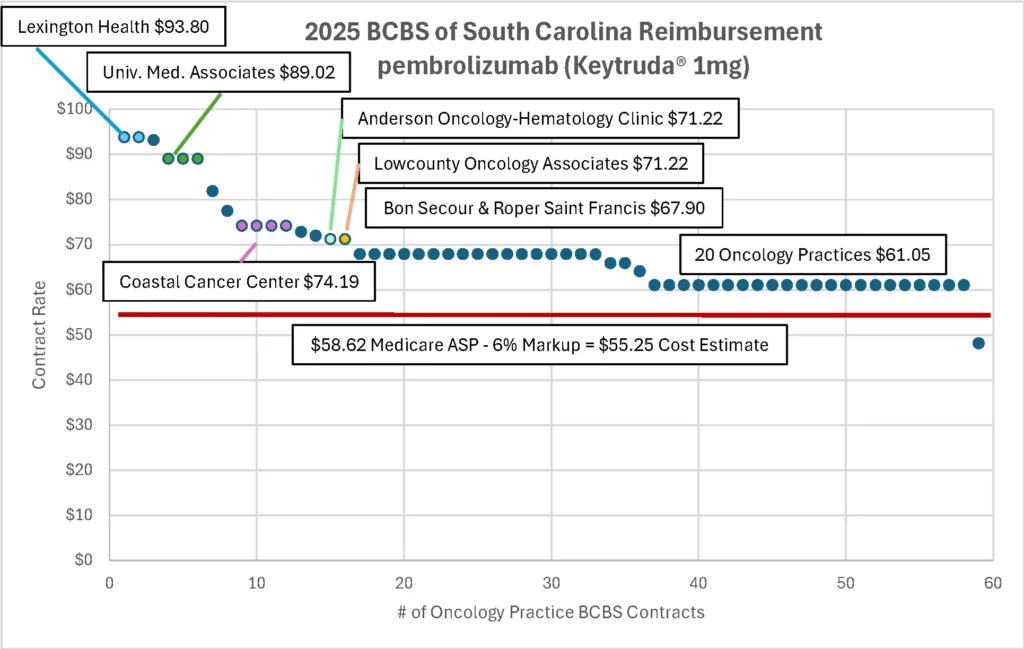
Example #1: BCBS of SC Keytruda® Reimbursement
Keytruda® was the #1 top selling drug in the world during 2024 and 2025. The graph below details commercial reimbursement rates under Blue Cross Blue Shield of South Carolina’s health plan for 1mg of pembrolizumab (Keytruda®) when administered in-office in oncology medical groups.
Given the standard dosage is 200 mg per treatment (200 times the contract amount below), medical groups in South Carolina net between $1,100 and $7,700 for each 30 minute infusion (reimbursement minus estimated costs). Infusions are typically given every three (3) weeks at this dosage.
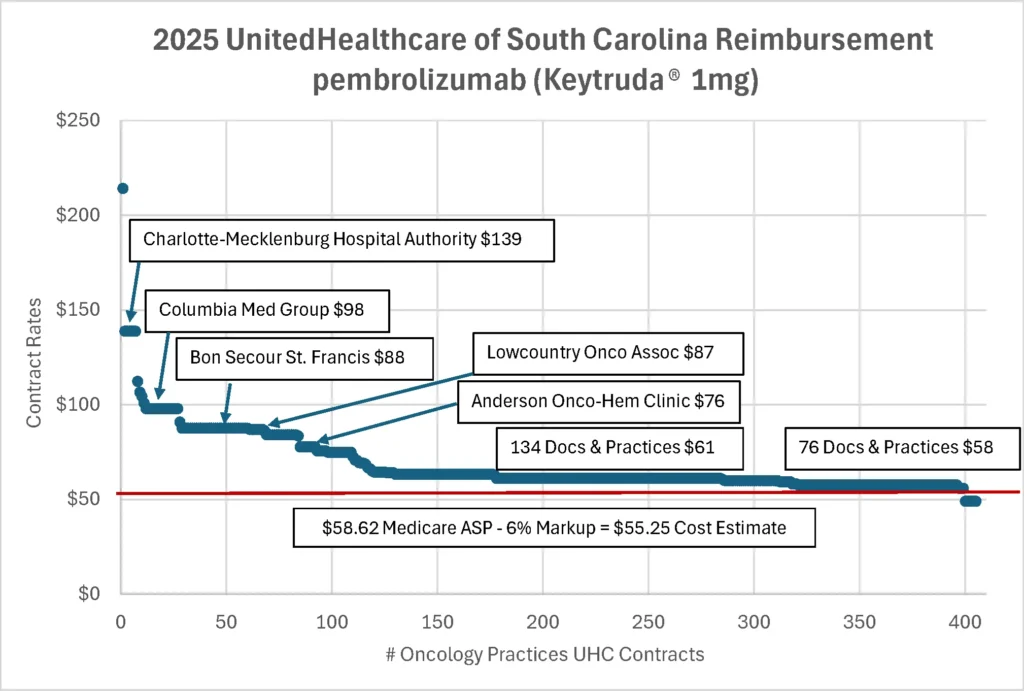
Example #2: UnitedHealthcare of SC Keytruda® Reimbursement
The graph below details commercial reimbursement rates under UnitedHealthcare of South Carolina’s health plan for 1 mg of pembrolizumab (Keytruda®) when administered in-office in oncology medical groups.
Given the standard dosage is 200 mg per treatment (200 times the contract amount below), medical groups in South Carolina net between $124 and $17,000 for each 30 minute infusion (reimbursement minus estimated costs). Infusions are typically given every three (3) weeks at this dosage.
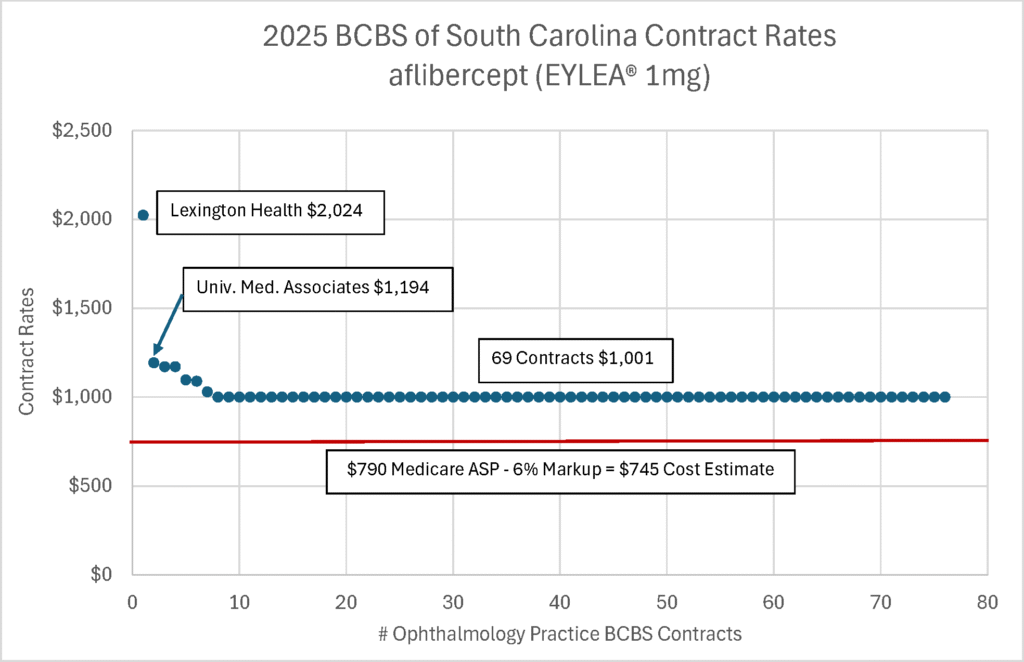
Example #3: BCBS of SC Eylea® Reimbursement
Eylea is the #1 drug administered by U.S. ophthalmologists in their offices (by total sales). The graph below details commercial reimbursement rates under Blue Cross Blue Shield of South Carolina’s health plan for 1mg of aflibercept (Eylea®) when administered in-office in ophthalmology medical groups.
Given the standard dosage is 2 mg per treatment (twice the contract amount below), medical groups in South Carolina net between $500 and $2,500 for each in-office injection (reimbursement minus estimated costs). Injections are typically given every month at this dosage for the initial 3 to 5 months. Maintenance injections are bi-monthly thereafter.
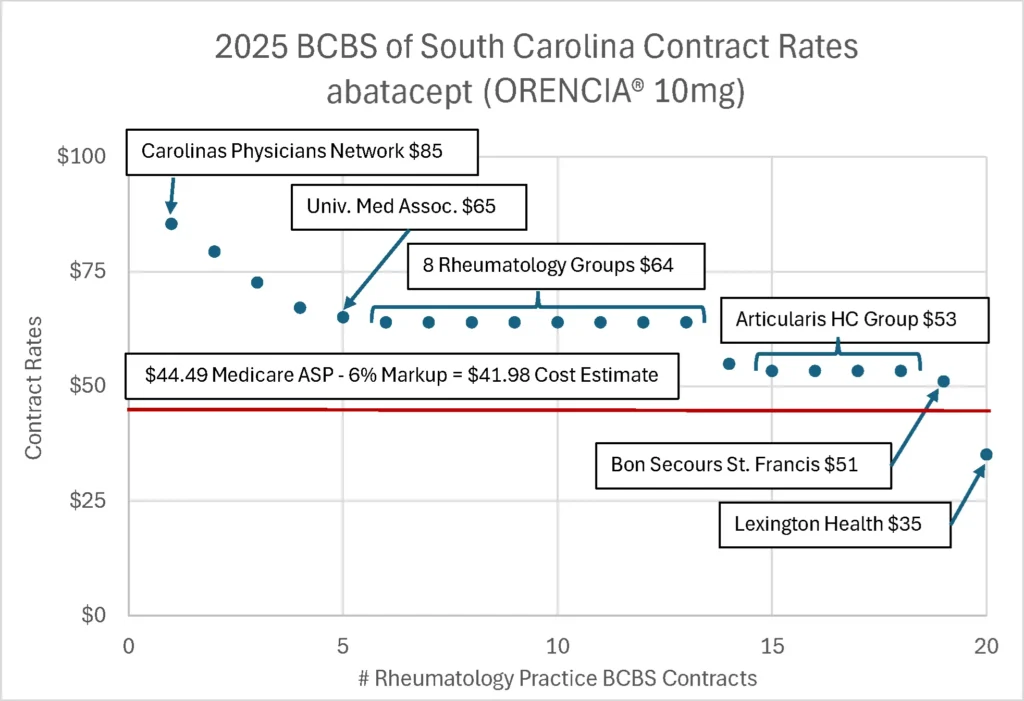
Example #4: BCBS of South Carolina Orencia® Reimbursement
Orencia® is the #1 drug administered by rheumatologists in their offices (by sales). The graph below details commercial reimbursement rates under Blue Cross Blue Shield of South Carolina’s health plan for 10mg of abatacept (Orencia®) when administered in-office in rheumatology medical groups.
Given the standard dosage ranges from 500 mg to 750 mg per infusion treatment (based on patient weight), medical groups in South Carolina net between $0 and $3,250 for each in-office infusion (reimbursement minus estimated costs). Infusions are typically given at the initial visit, then at 2 weeks, and then every 4 weeks thereafter. While some patients give themselves 125 mg injections at home, Orencia is still the most billed in-office drug administered by rheumatologists in the U.S. (by total sales).
Where does this data come from?
UnitedHealthcare, Cigna, Aetna, Elevance, and other commercial carriers released hundreds of thousands of massive data files (>100 GB per file) under the Transparency in Coverage rules. Unfortunately, these carriers released health plan data files in an obscure data format (json) that is difficult to parse. Most of these massive multi-gigabyte files cannot be opened in Microsoft Excel.
We do the hard programming work, so you don’t have to.
Do NOT pay more to FAIR Health or Optum for blinded data for one procedure code in one ZIP code.
Purchase prepaid Health Plan Query Credits.
Use these credits whenever you need them. These query credits never expire.
What is a Per Health Plan Query Credit? What does it get me?
Pricing is based on the number of unique health plans searched, not the number of drug or service codes searched. If you request searches on three (3) health plans, pricing does not change whether you request searches for one (1) service code or 100 service codes on those three health plans. Searching three health plans costs three credits.
Examples #1, #3, and #4 above could all be included in one query on one health plan (BCBS of South Carolina).
Queries are custom searches performed by an Acuvance professional upon request. Turnaround times will be quoted at order, but expect turnaround times of 24 to 72 hours for most query searches.
If there are more than 1 million results, your data will be accessible via a private online portal. The Unlimited Query Plan is subject to limitations on processing time (24 to 72 hours per health plan ordered).
