Medicare is dropping the payment hammer on skin substitute reimbursement in 2026. This post covers Medicare’s new skin substitute payment changes, as well as the implications this has on commercial reimbursement.
Medicare spending on skin substitutes used in wound care treatments grew about 4000% or 40 times from about $250 million during 2019 to over $10 billion during 2024. To curb this exponential growth, Medicare has enacted a new payment policy that takes effect January 1, 2026.
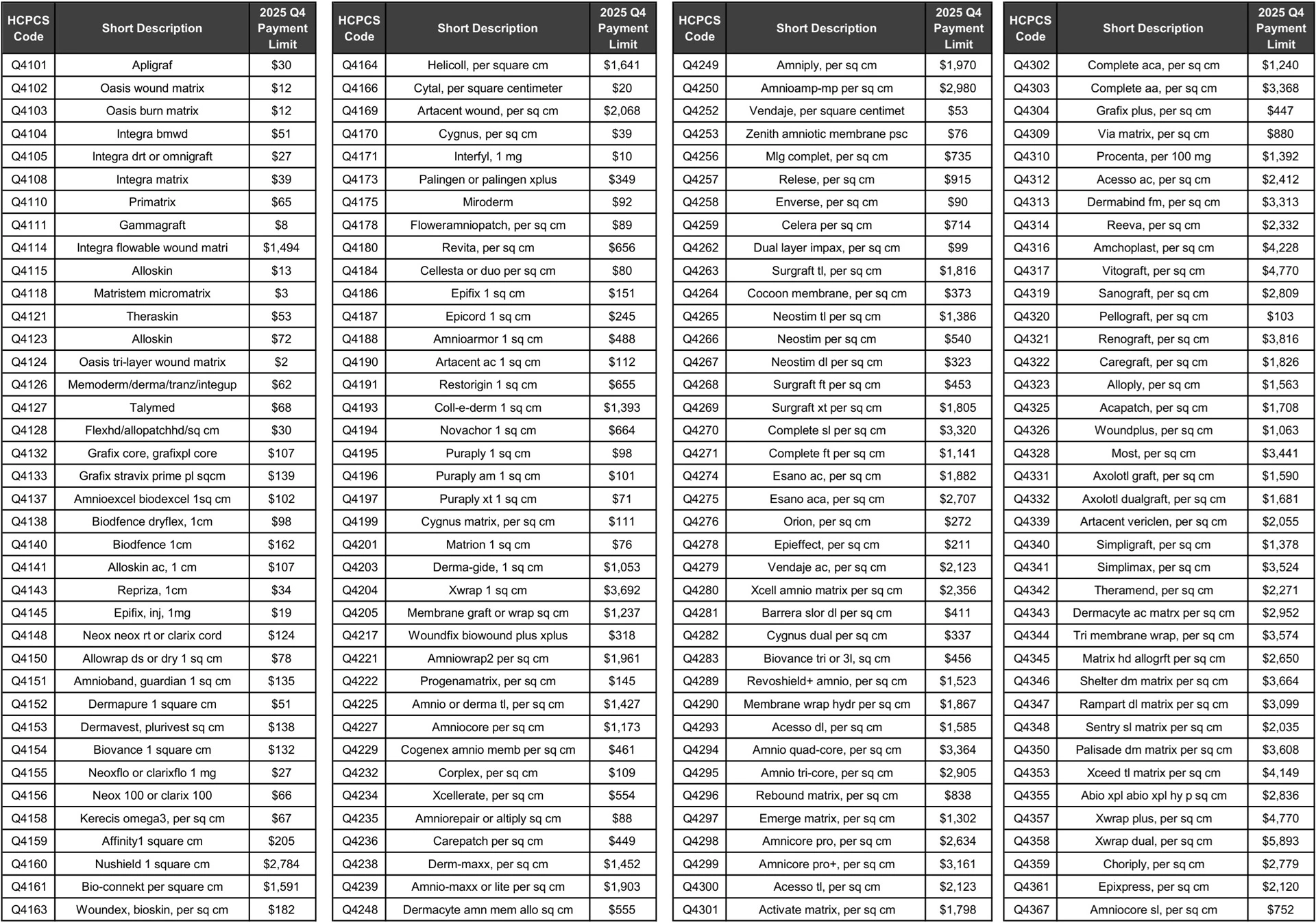
Up until now, skin substitutes were considered biologics payable under Medicare’s Average Sales Price or ASP methodology. But beginning in 2026, the 152 Q-codes for skin substitutes will be completely eliminated from Medicare’s ASP payment model.
Skin Substitute Deletions from Medicare ASP Model Effective January 1, 2026
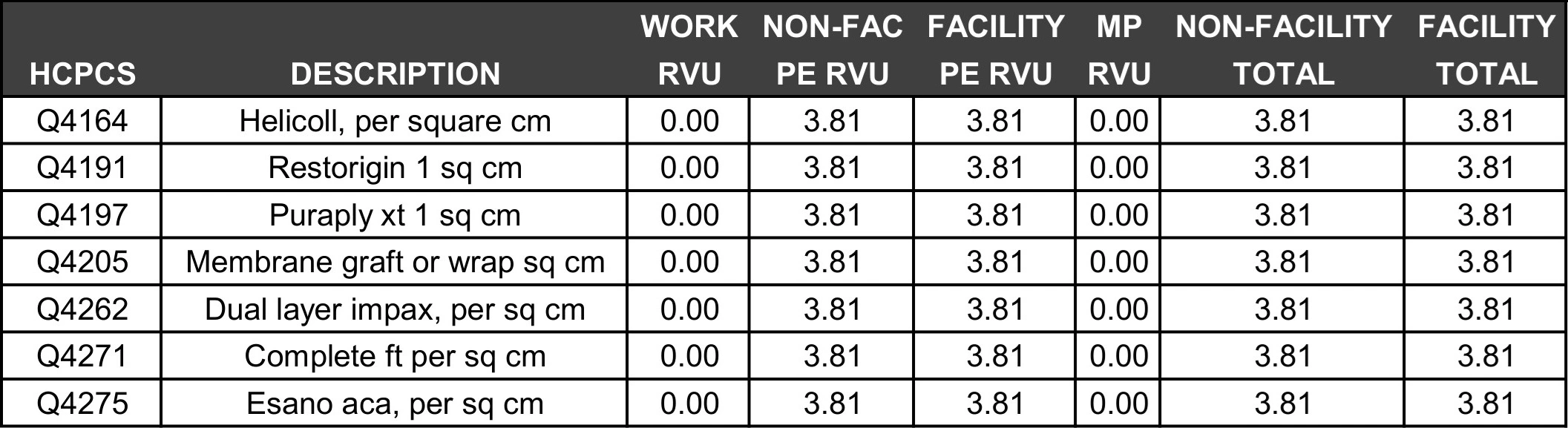
In 2026, Medicare is shifting skin substitute reimbursement to be add-on codes to physician application services using a single, flat payment rate of $127 per square centimeter across all 152 Q-codes. This means all 152 Q-codes for skin substitutes have moved from the ASP fee schedule to the Medicare physician fee schedule. All 152 Q-codes now have a non-facility practice expense relative value of 3.81 practice expense RVUs.
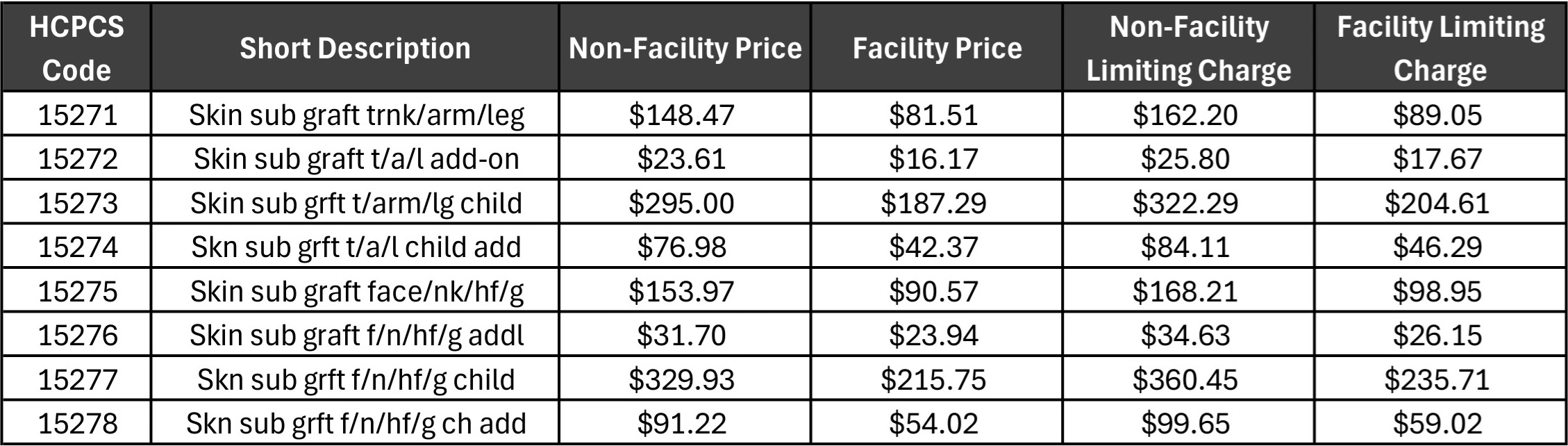
Sample of New Skin Substitute Incident-to-Supply Code Values (2026 MPFS)
Allegedly, some manufacturers were issuing large rebates to wound care providers that were not reflected in the Average Sales Prices or ASP reports those manufacturers provided to Medicare quarterly. This allegedly had the effect of pumping up skin substitute reimbursement while not reflecting the true sales costs after rebates were issued to provider organizations.
Obviously, the new standard rate of $127 per square centimeter is much less than the $1,000 to $2,000 per square centimeter sales prices that some manufacturers have allegedly been reporting during the past several years.
Medicare forecasts this change in payment policy will reduce program spending on skin substitutes nearly 90% and save Medicare billions of dollars. According to Medicare’s comment responses in the Federal Register, approximately 90% of these skin substitute services have been billed in non-facility office settings.
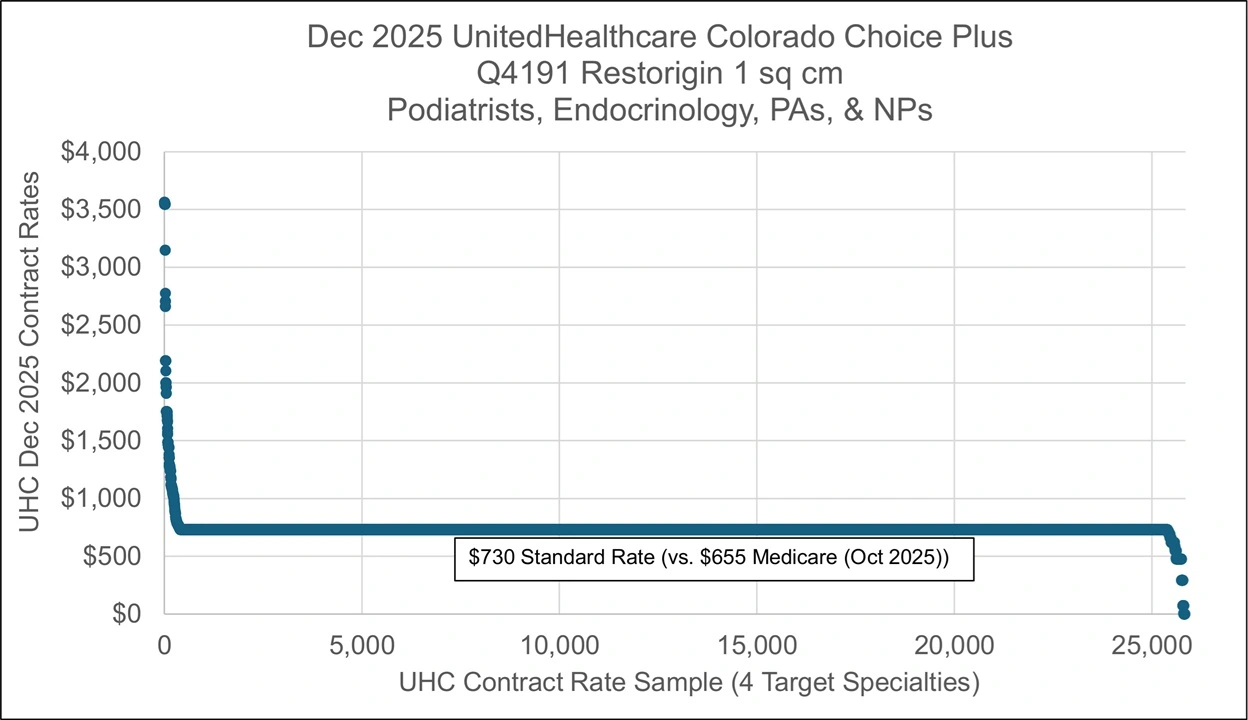
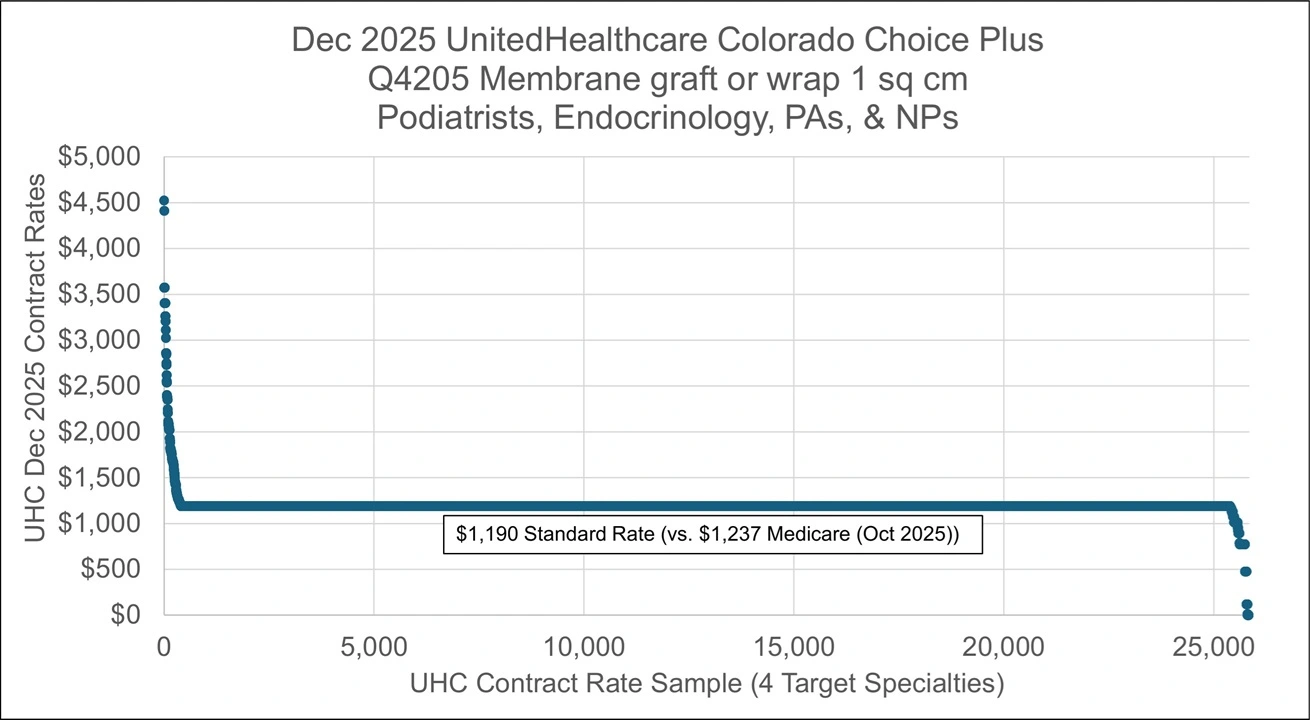
While the Medicare changes become effective January 1, 2026, it may be some time before all the commercial health plans respond. Commercial payers may have three year contracts, which means they could be locked into the old reimbursement rates until 2029. Additionally, while some commercial payors pay more than Medicare for skin substitutes, some commercial payors are already paying less than Medicare for skin substitutes.
UnitedHealthcare Dec. 2025 Colorado Skin Substitute Rate Examples
Lastly, going forward, payments for the skin substitute products are going to be billed as add-on codes to the professional physician application service fees. In non-hospital wound care centers, independent physicians must either buy skin substitutes themselves or subcontract with a management company to procure them. Physician practice management companies provide independent physicians with the facilities, support staff, and supplies (including skin substitutes) to provide patient care.
Skin Substitute Application Services Codes (2025 MPFS)