Congestive heart failure is one of the highest-cost diseases driving hospital readmissions and healthcare costs in the U.S. A highly effective treatment for preventing hospital readmissions of heart failure patients is intensive cardiac rehab. The intensive cardiac rehab benefits under Medicare and commercial payers pay physicians and hospitals surprisingly good reimbursement.
Congestive heart failure (CHF) is one of the most financially crippling chronic diseases for insurance companies, patients, and value-based care programs. Heart failure is one of the most common reasons for Medicare enrollees to be admitted to hospitals, and CHF patients are some of the most expensive of all health insurance enrollees. Multiple different studies and meta-analysis reviews indicate that the average annual healthcare costs for CHF patients are about $33,000 every year for each CHF patient.1,2 One study found per member per month costs for individuals with CHF to be over five times higher than individuals without CHF.
At a basic level, CHF occurs when a person’s heart pumps weakly or with a lack of adequate force. This causes fluid to back up in the lungs. CHF patients may feel shortness of breath and fatigue. The normal treatment involves drugs, particularly a water pill, which serves as a diuretic to drain off the excess water being held by the patient’s body. It is not unheard of for CHF patients to lose ten pounds of water or more during the initial days after starting a water pill.
While all this sounds pretty bad, CHF is actually very treatable, and the best treatments are extremely affordable. After all, the water pill is just a diuretic. The other treatment, cardiac rehabilitation, is a physician supervised program that furnishes physician prescribed exercise; cardiac risk factor modification, including education, counseling, and behavioral intervention; psychosocial assessment; and outcomes assessment.
Cardiac rehab is a medically supervised program for patients who have just had a heart attack, cardiac catheterization, coronary artery bypass graft, or other invasive heart surgery, or angina. Medicare covers up to 36 regular cardiac rehab sessions per year, or up to 72 intensive cardiac rehab sessions per year, if the patients are eligible under the aforementioned criteria during the past 12 months.
The core exercise component of cardiac rehab is usually walking on a treadmill or riding a stationary bicycle.
Intensive cardiac rehab programs furnish services more frequently and rigorously than “regular” cardiac rehab programs. Intensive cardiac rehab programs are lifestyle behavior modification programs that are funded by Medicare after CMS has reviewed and approved scientific evidence that each program is effective through the National Coverage Determination process.
The Dr. Ornish Program for Heart Disease Reversal, the Pritikin Program, and The Benson-Henry Institute Cardiac Wellness Program are the only three Intensive Cardiac Rehab programs currently approved.
Medicare and commercial insurance carriers pay higher reimbursement rates for a larger number of sessions for intensive cardiac rehab, in comparison to regular cardiac rehab.
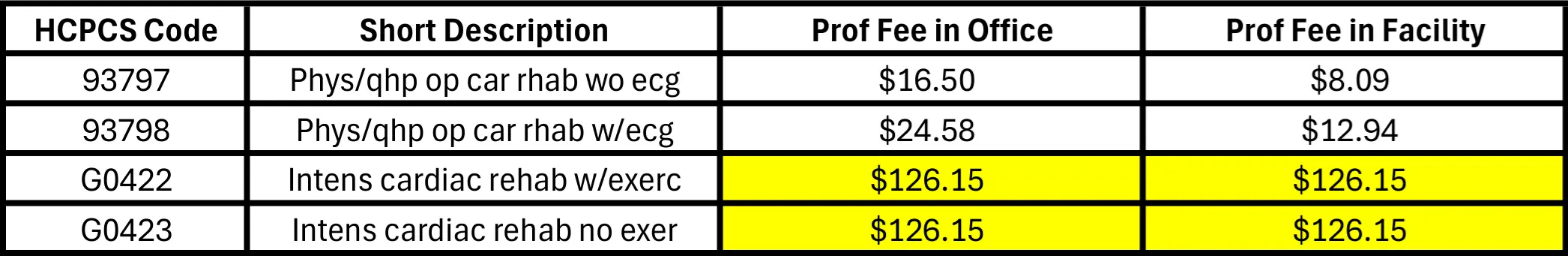
In outpatient hospital departments, Medicare pays hospitals about $126 for every session of cardiac rehab under APC code 5771, whether hospitals provide regular or intensive cardiac rehab. If cardiac rehab is conducted in a physician’s office, Medicare’s physician reimbursement is also $126 for intensive cardiac rehab, but only about $17 to $25 for each session of regular cardiac rehab.
2025 Medicare Professional Fees: Cardiac Rehab
Under Medicare’s intensive cardiac rehab benefit, both the physician and a hospital department would each receive $126 for each patient session in a hospital outpatient department, or about $250 in total. Cardiac rehab can be administered in groups or classes, involving many patients at one time. Because intensive cardiac rehab providers can treat several patients at once, there are great opportunities for this to be a profitable service line.
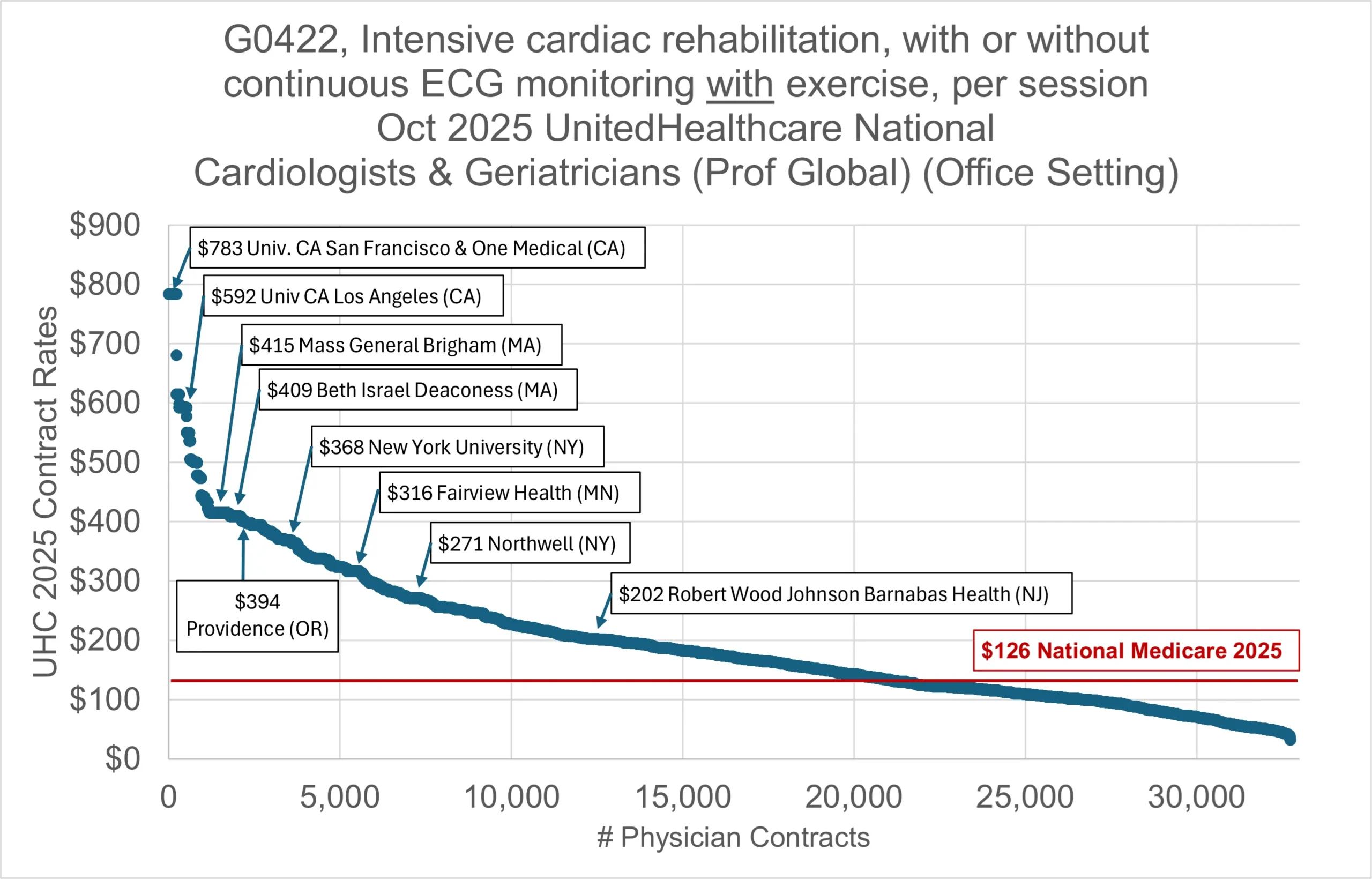
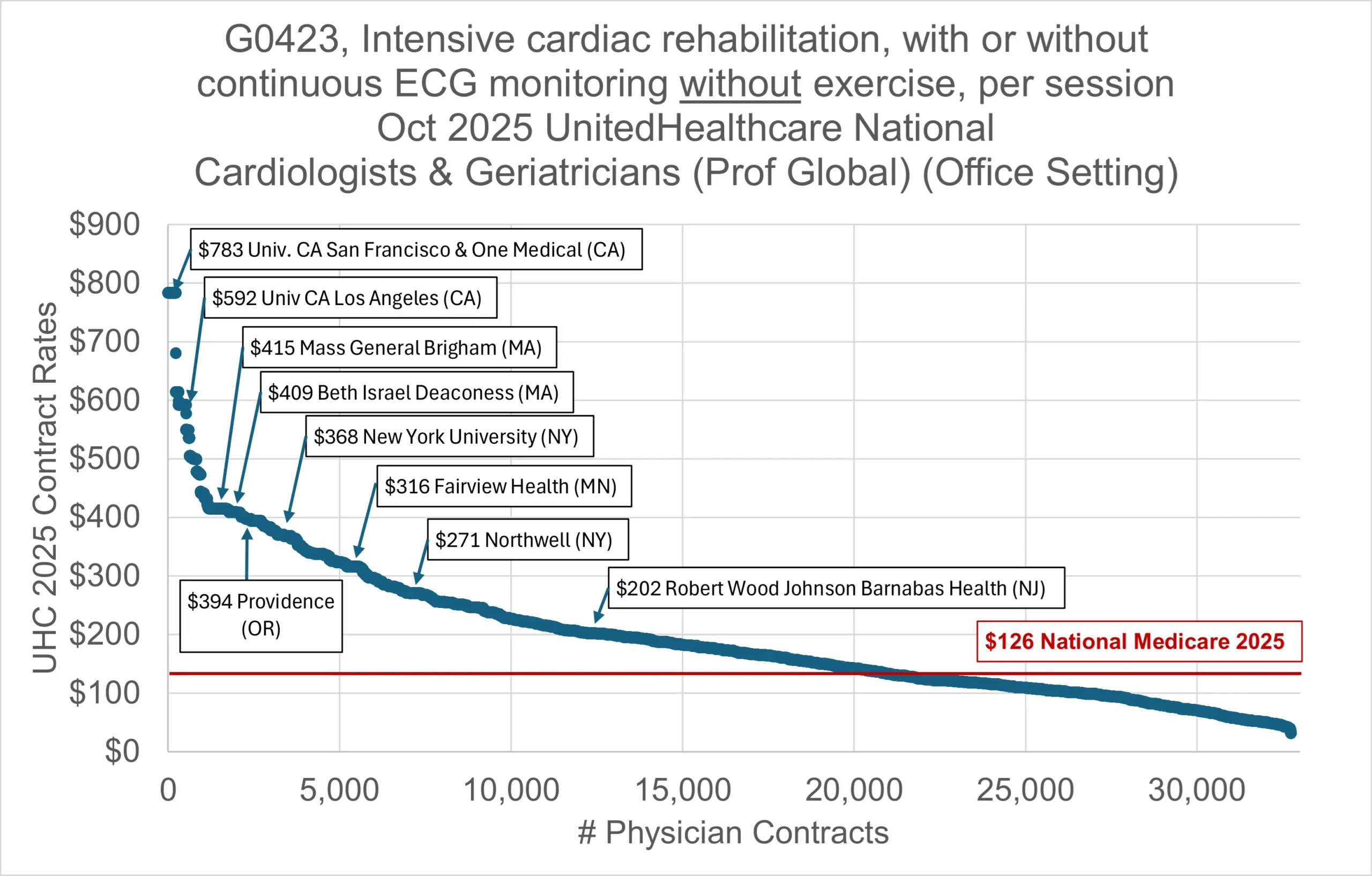
Commercial insurance carriers may pay substantially more than Medicare for cardiac rehabilitation. 2025 data from UnitedHealthcare indicates that it regularly pays cardiologists markups on Medicare from 40% to well over 300%.
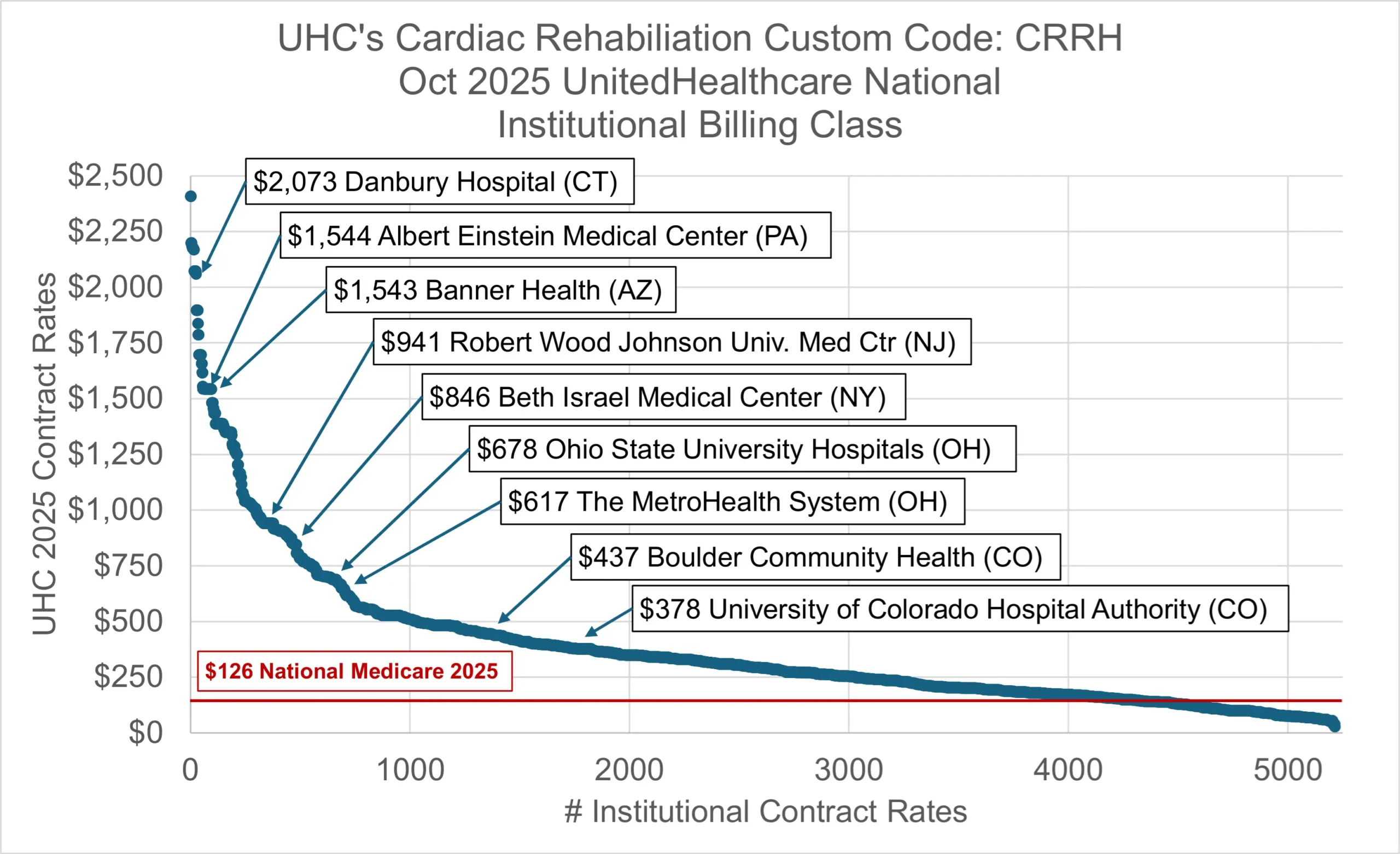
Apart from professional physician fees, many hospital outpatient facilities also receive much higher reimbursement from commercial payers than Medicare. UHC’s median institutional facility rate nationwide is about 200% of the Medicare APC rate for the same service. Some hospital outpatient departments receive 300% to 1000% of Medicare’s hospital APC rate or more.
2025 UnitedHealthcare Professional Fees: Intensive Cardiac Rehab
2025 UnitedHealthcare Facility Fees: Cardiac Rehab
The approved intensive cardiac rehab programs were developed privately and may require special training, licenses, or accreditations. For example, in 2014, Dr. Dean Ornish licensed the exclusive rights to his heart disease treatment program to the company Healthways. All hospitals and physician practices that wanted to use Dr. Ornish’s Program for Reversing Heart Disease had to get accredited from Healthways in order to bill Medicare and commercial payers for this service. Healthways sold the license to the company Sharecare during 2016.
Multiple meta-analyses of hundreds of studies have indicated that cardiac rehab is arguably one of the most cost-effective treatments available for reducing hospital re-admissions.3,4,5
Despite compelling evidence of the benefits of cardiac rehab to patients, treatment adherence is stunningly low, especially for CHF patients. Multiple studies have cited only 3% to 5% of patients engage in cardiac rehab after an initial diagnosis of CHF.6,7,8 The most commonly cited barriers to treatment include distance from the program facility; transportation; low patient self-esteem; and lack of physician referral, perceived benefit, and social support.9
Fortunately, there are several new Value-Based Care exceptions to the Stark Law that support innovative ways to engage patients and physicians in services like cardiac rehab. Providers that fulfill the new Stark exceptions can provide patients with support services that encourage treatment adherence. For example, if the VBE exception is fulfilled, patients may be eligible for transportation to cardiac rehab to support their adherence to treatment. Similar patient incentive waivers that support treatment adherence are afforded to Accountable Care Organizations participating in the Medicare Shared Savings Program.
Are you interested in reimbursement for medically supervised cardiac rehab?
Do you need help reducing hospital readmissions?
Sources:
- Expenditure on Heart Failure in the United States: The Medical Expenditure Panel Survey 2009-2018. JACC: Heart Failure. Volume 10, No. 8. July 6, 2022.
https://www.jacc.org/doi/10.1016/j.jchf.2022.05.006#:~:text=In%20the%20United%20States%2C%20an,with%20HF%20was%20$179.5%20billion. - Chen Wei, Paul A. Heidenreich, Alexander T. Sandhu. The economics of heart failure care. Progress in Cardiovascular Diseases. Volume 82, January–February 2024, Pages 90-101.
- Smart N, Marwick TH. Exercise training for patients with heart failure: a systematic review of factors that improve mortality and morbidity. Am J Med. 2004 May 15;116(10):693–706.
- Morris JH, Chen L. Exercise Training and Heart Failure: A Review of the Literature. Card Fail Rev. 2019 Feb;5(1):57-61. doi: 10.15420/cfr.2018.31.1. PMID: 30847247; PMCID: PMC6396064.
- Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalal HM, Lough F, Rees K, Singh S, Taylor RS. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. Open Heart. 2015 Jan 28;2(1):e000163. doi: 10.1136/openhrt-2014-000163. PMID: 25685361; PMCID: PMC4316592.
- Pandey, A, Keshvani, N, Zhone, L. Temporal Trends and Factors Associated With Cardiac Rehabilitation Participation Among Medicare Beneficiaries With Heart Failure. JACC: Heart Failure. Volume 9, Issue 7, July 2021, Pages 471-481.
- American Heart Association Quality of Care & Outcomes Research Meeting Report, Presentation MDP7. https://newsroom.heart.org/news/less-than-10-of-adults-with-heart-failure-get-cardiac-rehab-despite-medicare-expansion
- Michigan Value Collaborative: 2023 Cardiac Rehab Report. https://michiganvalue.org/mvcs-2023-cardiac-rehabilitation-reports-shared-with-hospitals/
- Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs. 2002; 17(1):8–17.